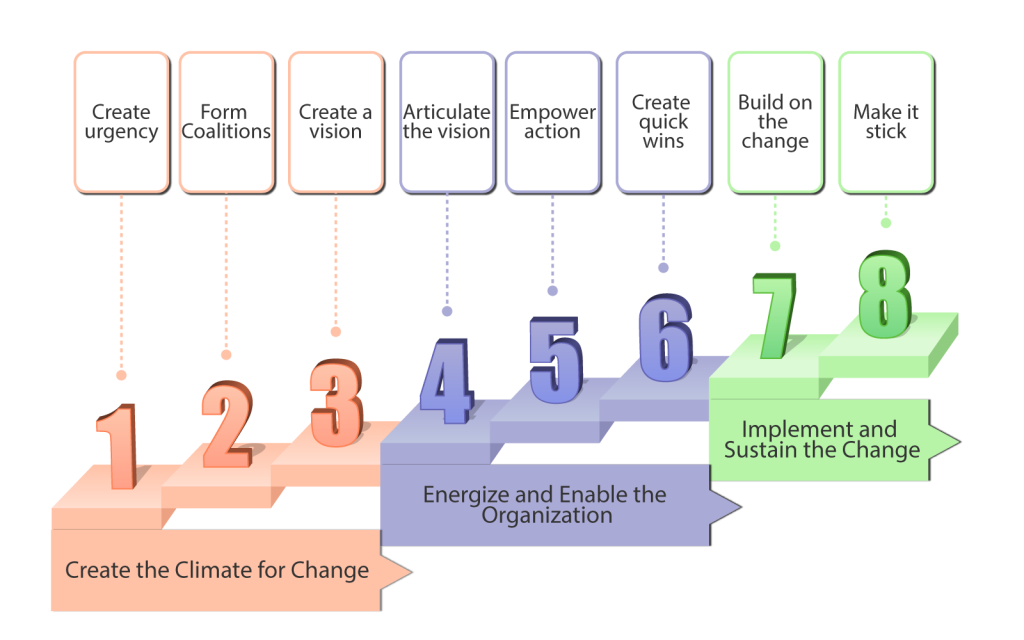
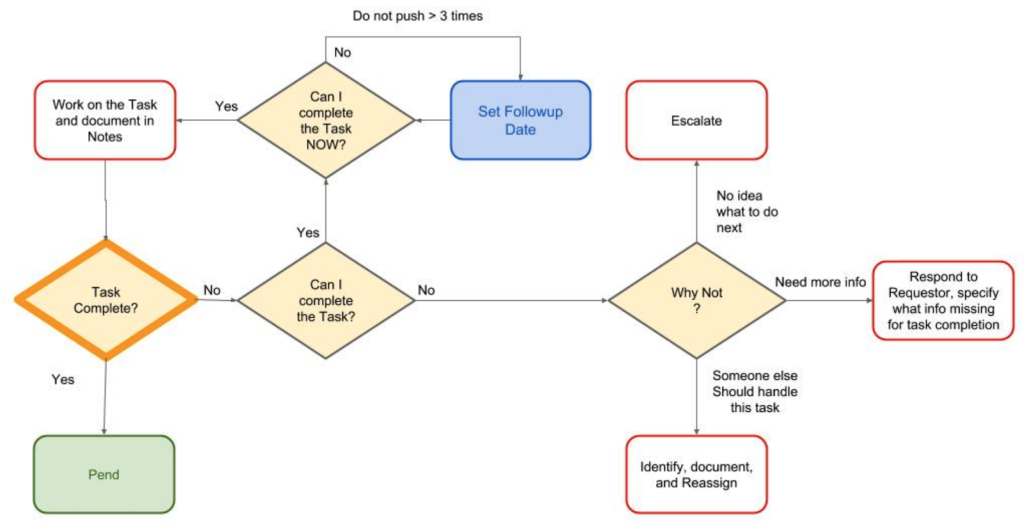
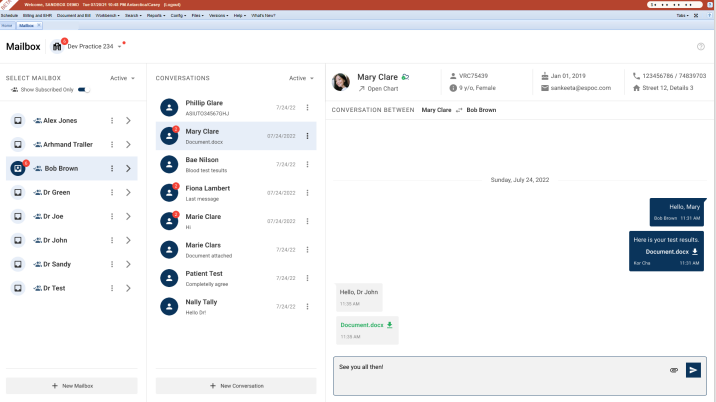
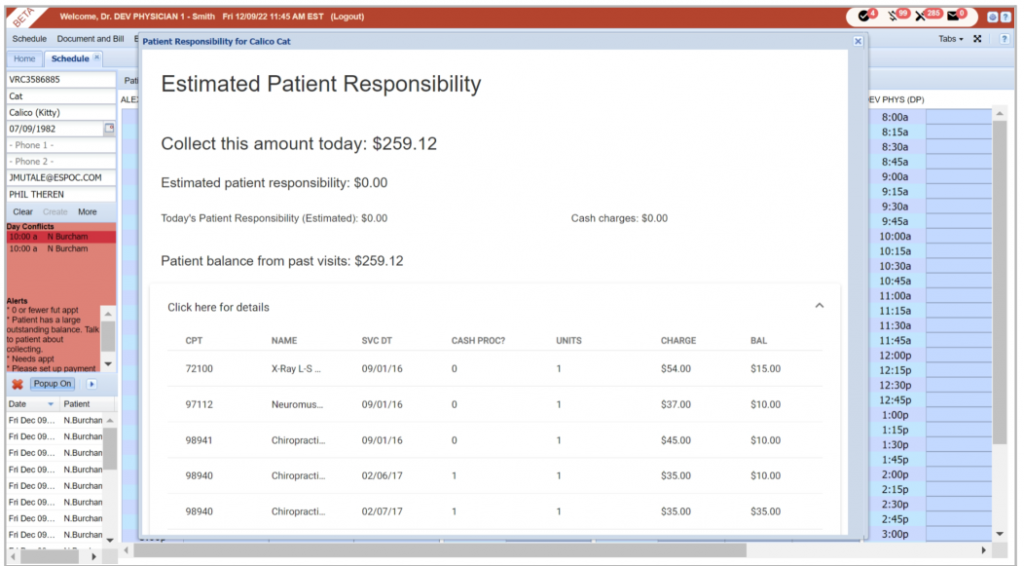
Medical billing complexity and massive volumes of daily claims render manual claims processes incapable of protecting both the provider and the payer from underpayments, overpayments, and billing compliance violations. Straight-Through Billing (STB) addresses complexity and volume processing problems by automating the majority of the claim flow and focusing the billing follow-up specialists on exceptions only. An STB process flags problems, routes them for follow-up, and enables online correction and resubmission. The STB methodology implements billing service transparency and focuses management on strategic process improvement opportunities. Straight-Through Billing integrates the billing process into the practice management workflow, automates the vast majority of transactions, focuses manual labor on exceptions, and establishes a process for continuous improvement. Remember: Straight-Through Billing offers a comprehensive approach to improving the billing process, integrating various components, and promoting continuous improvement. Practice Management Integration First, integrated practice management and billing workflow connects patient scheduling, medical record management, and billing into a single process. Every participant in the practice management workflow receives a unified and coherent picture of the practice workload, patient and provider location, resource availability, and cash flow. However, integrated with Electronic Health Records, practice management systems are more beneficial. Electronic health records (EHR) are digital formats of a patient’s chart. They contain all the information about a patient’s health. This includes medical history, allergies, immunizations, previous treatments, medication history, past diagnoses, history of substance abuse (if any), and so forth (Shah, 2021). Transaction Automation Transaction automation streamlines and expedites the billing process by automating claim validation, payer message reconciliation, and billing workflow management: Automated claim validation eliminates errors downstream and reduces processing time because it flags errors before submitting the claim to the payer. Automated claim message reconciliation eliminates the costly search for the original claim and standardizes message communication, eliminating the need to decipher the (often cryptic) payer’s message. Automated billing workflow management drives the follow-up discipline required for the resolution of claim denial and underpayment incidents, and it establishes a high degree of process transparency for all billing process participants, resulting in full and timely payments. Automated billing increases the net collection rate due to quick claim turnaround and efficient follow-up. Respond to your denials within 5-21 business days of receiving them, using our Daily Denial Email Alerts (Qureshi, 2022). Focus on Exceptions Focusing manual labor on exceptions requires timely exception identification, routing to follow-up personnel, online error correction, and rigorous follow-up tracking. Again, process transparency enables tracking exception follow-up as implemented in ClinicMind-like systems. Another significant benefit of automated medical billing is the ability to track and analyze financial data. With this, healthcare facilities can monitor their revenue cycles, identify growth opportunities, and generate detailed financial reports (Polo, 2023). Continuous Process Improvement Finally, a process for continuous improvement requires continuous observability of every process attribute and a modification methodology for both automated claim processing and manual exception follow-up tracking. Straight-Through Billing implements billing transparency by design because billing transparency is an integral attribute of every component of the STB process. It also enables businesses to streamline their billing operations, reduce errors, enhance efficiencies, and improve the customer experience (Ward, 2023). Straight-Through Billing Architecture The Straight-Through Billing systems architecture mirrors the architecture of general Straight-Through Processing (STP) systems developed for the financial services industry. Such systems require effective workflow management, a knowledge-based validation system, connectivity to all process participants (including online data reconciliation), and tracking of problem resolution. Therefore, a typical ClinicMind-like STB system has a three-tiered architecture: Back-end processing engine, designed for a high-volume transaction processing environment Middle tier, using Java Servlet technology Front end, using an HTML-JavaScript, zero-footprint client Did You Know? The STB architecture is inspired by the systems used in the financial services industry, showcasing the transferability of advanced processing concepts across different domains. An STB system (e.g., ClinicMind) based on the methodology outlined here implements rich functionality, which allows the following to be automated: Computer-aided preferential patient scheduling Integrated electronic medical records Online computer-aided coding Real-time claim validation and patient eligibility testing Electronic claim submission Payment posting, reconciliation, and verification of meeting contractual obligations Monitoring of audit risk and billing compliance Tracking of denial appeal process Quantitative STB Management Straight-Through Billing methodology allows for quantitative management since the likelihood of the entire process failing can be estimated as the product of such items for each individual workflow step. A ClinicMind-like STB system tracks the percentage of clean claims (claims paid in full, and within the allocated time frame, without any manual intervention) and focuses the management on those process aspects that yield the greatest potential improvement. Thus, STB methodology focuses on exceptions at both the tactical and strategic management levels and can help to improve cash flow and reduce outstanding invoices by providing real-time visibility into billing and payment status (Mielnicki, 2022). Modern Insights and Research In the ever-evolving field of medical billing, staying ahead of the curve is crucial for achieving financial excellence in the healthcare industry. Let’s embark on an exhilarating journey into the future of medical billing, where the convergence of electronic health records (EHRs), artificial intelligence (AI), real-time analytics, and collaborative efforts reshapes the revenue cycle landscape. Brace yourself for a transformative exploration that revolutionizes processes, enhances data accuracy, maximizes financial outcomes, and ushers in an era of unparalleled efficiency and effectiveness in the dynamic realm of medical billing. 1- Role of Blockchain Technology in Billing Systems The seamless integration of electronic health records (EHRs) and billing systems is revolutionizing the field of medical billing. Gone are the days of fragmented medical records scattered across various healthcare organizations. With blockchain at the helm, a distributed EHR ecosystem emerges, ensuring a smooth flow of information between providers. By eliminating manual data entry and ensuring accurate documentation, this innovative technology guarantees accurate and secure documentation, eliminating errors and speeding up reimbursement processes (Cerchione et al., 2022). But that’s not all. Blockchain brings an unparalleled level of data integrity and security, employing cryptographic techniques to safeguard patient information from prying eyes.

AI in Medical Billing
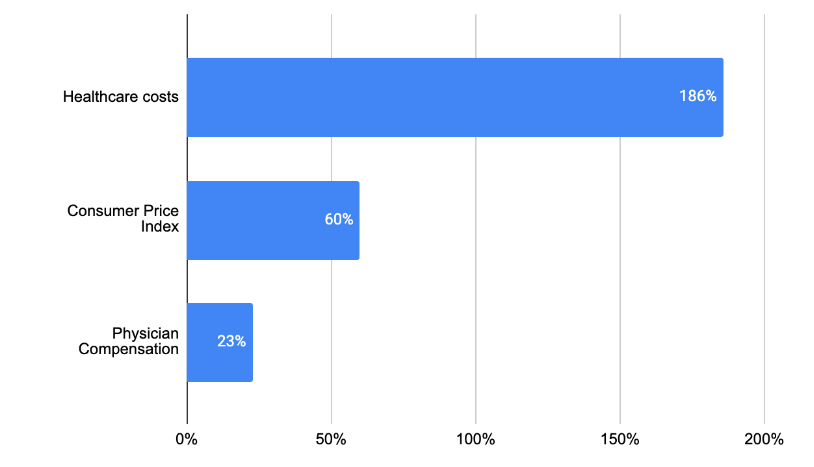
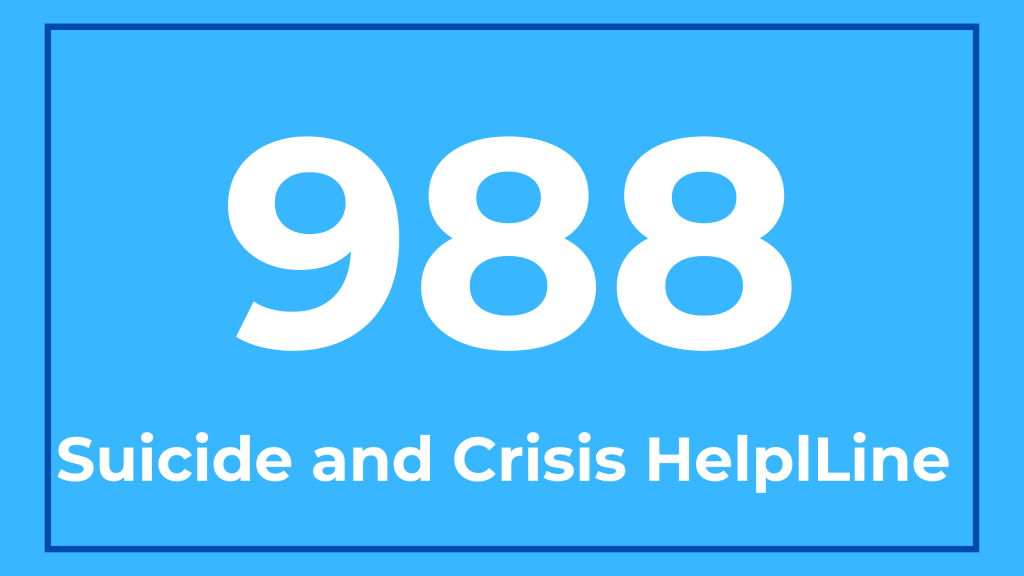
AI has revolutionized many different industries, and healthcare is no exception. In recent years, medical billing has benefited greatly from using Artificial Intelligence. Where are the major pain points in healthcare today? 1-Patients: A major challenge today is long wait times. In 2022, the average wait time for a physician appointment in the 15 largest U.S. metro markets is 26 days [1]. The longer someone has to wait, the higher the risk of complications or possibly more serious health issues arising. Some possible solutions to address this problem include use of telemedicine involves providing medical consultations and services remotely using technology such as video conferencing. increasing the number of healthcare professionals in practice, streamlining administrative processes and improving patient communication and education to help prevent avoidable illnesses and hospital visits. 2-Physicians: Physician burnout is affecting a high percentage of physicians. 62.8% of physicians experienced at least one